Incidence of IONM Data Changes Due to Patient Positioning in 4,577 surgeries
February 07, 2018
INTRODUCTION:
Patient positioning during various types of surgeries may cause stretching, compression or ischemia of the peripheral nerves. Upper extremity nerves are more at risk than lower extremity nerves, resulting in postoperative neuropathy. Somatosensory evoked potentials (SSEPs) and transcranial motor evoked potentials (TCeMEPs) can be beneficial in identifying positioning issues. Repositioning the limb can prevent nerve damage from occurring.
METHODS:
We retrospectively reviewed 4,577 surgeries performed with neurophysiological monitoring during 2016 and 2017. The total patients consisted of 53% female and 47% male. IONM data changes related to positioning were identified in 142 of the patients. Of the 142 patients, 61 were female (43%) and 81 were male (57%) with ages ranging from 19 to 86 years (median: 59 years). We utilized SSEPs, TCeMEPs, and spontaneous EMG from all four extremities. Train of four (TOF) was recorded from the abductor hallucis muscle for monitoring the level of muscle relaxant.
RESULTS:
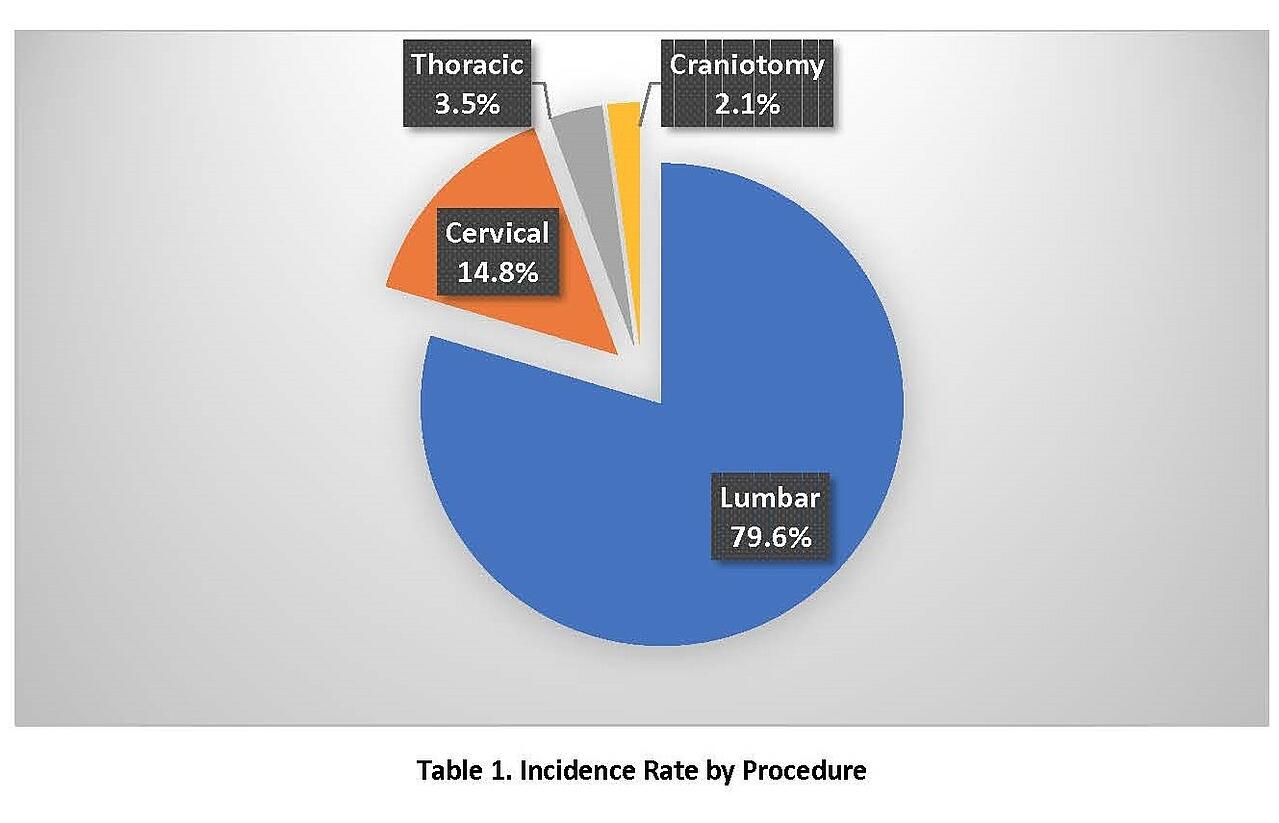
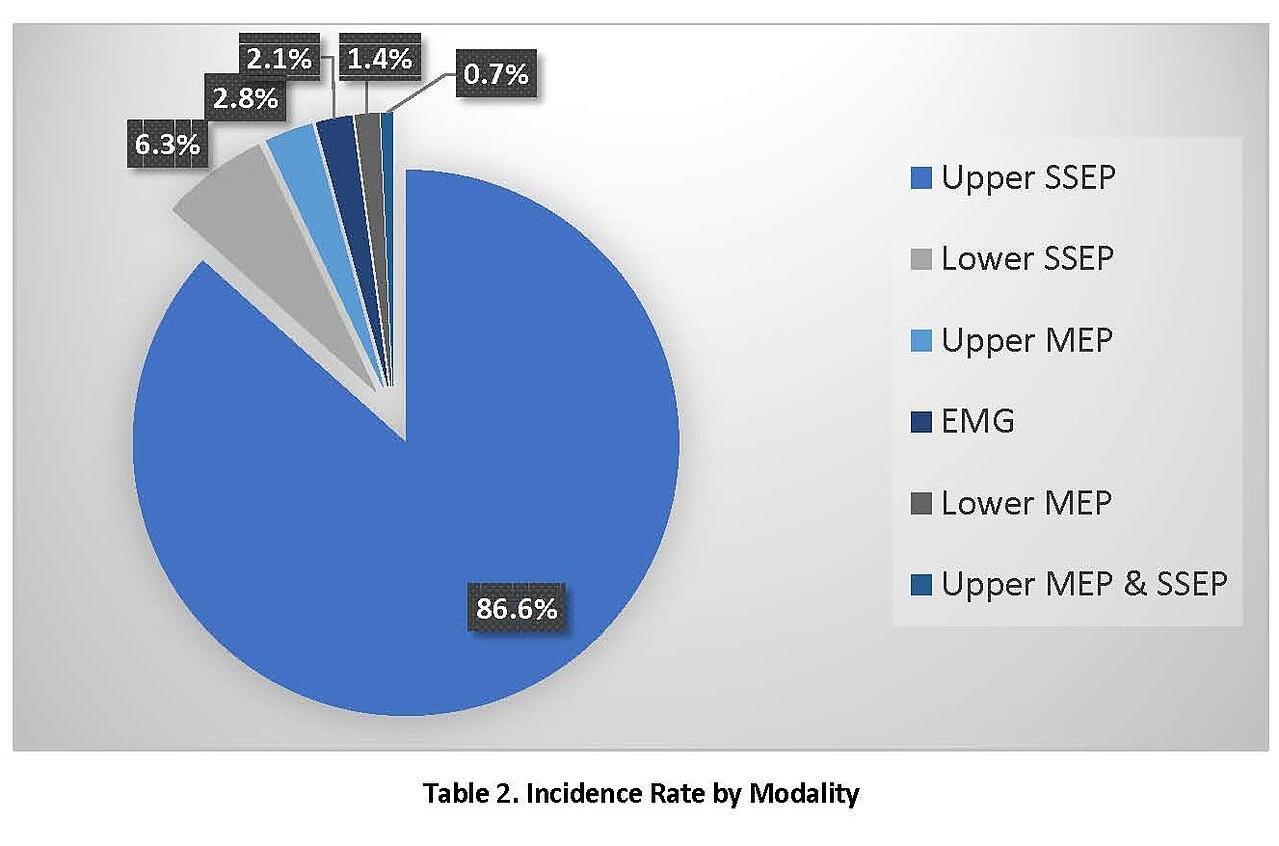
We identified 142 cases with changes in neurophysiological data due to patient positioning out of 4577 total surgeries. The total incidence of positioning effects was 3.1%. The signals returned to baseline with repositioning in 72.5% of the surgeries. The highest incidence of change was observed in lumbar surgery (79.6%), followed by cervical surgery (14.8%), thoracic surgery (3.5%) and craniotomy (2.1%). The highest incidence of change was observed in upper SSEP data (86.6%), followed by lower SSEP data (6.3%), upper MEP data (2.8%), spontaneous EMG activity (2.1%), lower MEP data (1.4%), and upper MEP and SSEP data (0.7%). We observed that 65.5% of the changes identified were in upper SSEPs during lumbar surgery.
CONCLUSIONS:
Intraoperative multimodality IONM is a protective tool against neuropathy and positioning complications during various surgical procedures. We highly recommend monitoring upper SSEPs for lumbar surgery due to the correlated incidence rate. Early identification of changes in SSEP, TCeMEP, and sEMG signals during surgery can detect positioning issues. This allows for intraoperative repositioning, thus minimizing post-operative neurological deficit.
Kathryn Overzet, MS, CNIM1,
Faisal R. Jahangiri, MD, CNIM, D.ABNM, F.ASNM1,
1 Axis Neuromonitoring LLC, Richardson, TX, USA.
Learn more about AXIS Neuromonitoring by downloading the brochure:
↓




