Minimizing Neurological Deficits by Electromyography (EMG) Monitoring during Lateral Lumbar Spine Surgeries
November 27, 2019
Faisal R. Jahangiri, M.D., CNIM, D.ABNM, FASNM, FASET1, Eloise Faust, CNIM1
1Axis Neuromonitoring LLC, Richardson, Texas, USA;
A 55-year-old female with history of low back pain, bilateral leg pain, and bilateral leg numbness with weakness was admitted with spondylolysis, spinal stenosis with neurogenic claudication, and intervertebral disc displacement. Co-morbidities included a history of hypertension, diabetes, hypothyroidism, Hasimoto’s, and high cholesterol.
Magnetic Resonance Imaging (MRI) of the patient’s lumbar spine revealed severe spinal stenosis at L3-L4/L4-L5 levels and spondylolisthesis at L4-L5 level. The surgeon decided to proceed with a two level Lateral Lumbar Interbody Fusion (LLIF) procedure at the L3-L4 and L4-L5 levels to treat the patient.
A multimodality Intraoperative Neurophysiological Monitoring (IONM) protocol was planned to include bilateral ulnar nerve, saphenous nerve and posterior tibial nerve Somatosensory Evoked Potentials (SSEPs) [1], bilateral upper and lower limb Transcranial electrical Motor Evoked Potentials (TCeMEPs), bilateral lower extremity EMG and Train of Four (TOF). Utilization of TCeMEP during posterior lumbar procedures has been reported in recently published literation for avoiding direct nerve injuries resulting in a foot drop [2,3,4]. The spontaneous (s-EMG) and triggered EMG (t-EMG) was also included to identify any nerve roots in the exposed area to prevent any nerve injuries.
The procedure was performed by a fellowship-trained orthopedic spine surgeon, with a CNIM [5] certified technologist providing the neuromonitoring in the operating room, and a D.ABNM [6] board-certified neurophysiologist available via remote-monitoring. A board-certified neurologist with a specialty in IONM was also present online for remote monitoring during the entire surgical procedure [7].
During placement of the lateral retractors, triggered EMG elicited responses at very low threshold in adductor brevis, vastus lateralis and rectus femoris muscles muscles (Figure). The surgeon was immediately alerted about the low threshold t-EMG responses. The surgeon repositioned the retractor blades. Stimulation by t-EMG was performed again which still elicited responses in the left thigh muscles. The surgeon decided that it was unsafe to proceed with the lateral procedure.
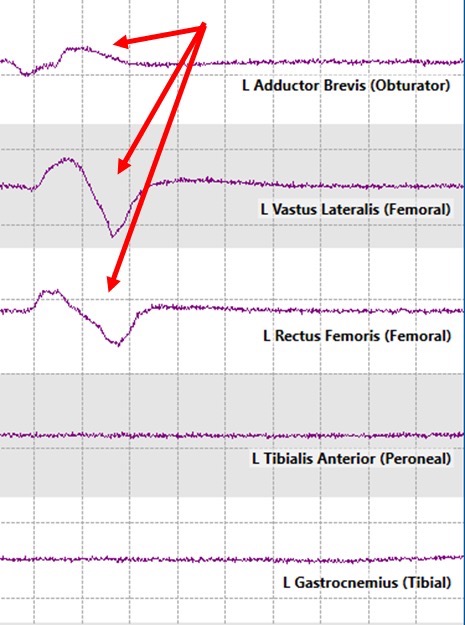
Figure: Triggered EMG (t-EMG) responses recorded in the left adductor brevis, vastus lateralis and rectus femoris muscles (red arrows).
Postoperatively, the patient had no neurological deficits due to early identification of low threshold t-EMG responses as well as quick intervention. If low threshold was not identified by intraoperative neuromonitoring, it may have resulted in a damage to the spinal nerves. Hence, patient would have post-operative thigh muscle weakness, numbness, severe pain, etc.
References
- American Clinical Neurophysiological Society. (2009). https://www.acns.org/pdf/guidelines/Guideline-11B.pdf. Retrieved May 29, 2019, from ACNS. Guideline 11B: Recommended standards for intraoperative monitoring of somatosensory evoked potentials: https://www.acns.org/pdf/guidelines/Guideline-11B.pdf
- Wilent, W. T.-Z. (2019). Utility of motor evoked potentials to diagnose and reduce lower extremity motor nerve root injuries during 4,386 extradural posterior lumbosacral spine procedures. The Spine J. doi:10.1016/j.spinee.2019.08.013
- Lieberman JA, L. R. (2019, Mar). The reliability of motor evoked potentials to predict dorsiflexion injuries during lumbosacral deformity surgery: the importance of multiple myotomal monitoring. Spine J, 19(3), 377-385. doi:10.1016/j.spinee.2018.07.006
- Tamkus A, R. K. (2018, Feb). Transcranial motor evoked potential alarm criteria to predict foot drop injury during lumbosacral surgery. Spine, 43(3), E227-E233. doi:10.1097/BRS.0000000000002288
- ABRET Neurodiagnostic Credentialing and Accreditation. (2019, Sep 9). ABRET. Retrieved Sep 9, 2019, from ABRET: https://www.abret.org/candidates/credentials/cnim/
- ABNM: American Board of Neurophysiologic Monitoring. (2019, Sep 9). ABNM: American Board of Neurophysiologic Monitoring. Retrieved Sep 9, 2019, from ABNM: American Board of Neurophysiologic Monitoring: http://www.abnm.info/
- Gertsch JH, Moreira JJ, Lee GR, Hastings JD, Ritzl E, Eccher MA, Cohen BA, Shils JL, McCaffrey MT, Balzer GK, Balzer JR, Boucharel W, Guo L, Hanson LL, Hemmer LB, Jahangiri FR, Mendez Vigil JA, Vogel RW, Wierzbowski LR, Wilent WB, Zuccaro JS, Yingling CD; membership of the ASNM. (2019). Practice guidelines for the supervising professional: intraoperative neurophysiological monitoring. J Clin Monit Comput, 33(2), 175-183. doi:10.1007/s10877-018-0201-



