Motor Evoked Potential (TCeMEP) Recordings from Urethral Electrodes
March 25, 2018
(Paper was presented by Dr. Faisal Jahangiri at the 2018 annual meeting of American Society of Neurophysiological Monitoring (ASNM) on Feb. 24, 2018 in Orlando, Florida. It received Second Place Scientific Achievement Award from the ASNM research committee).
INTRODUCTION:
Multimodality Intraoperative Neurophysiological Monitoring (IONM) is routinely performed during resection for tumors of the conus, cauda equina and nerve roots. Bowel and bladder function are at risk during these procedures and are usually only monitored with EMG and/or motor evoked potentials (MEP) recorded from the external anal sphincter muscles (EAS). Unfortunately, a narrow view of pelvic floor function is provided when only analyzing the EAS which does not include the monitoring of direct bladder function. This study demonstrates the ability to acquire MEPs from the urethral sphincter muscles (USMEP) by utilizing a urethral catheter with an electrode attached.
METHODS:
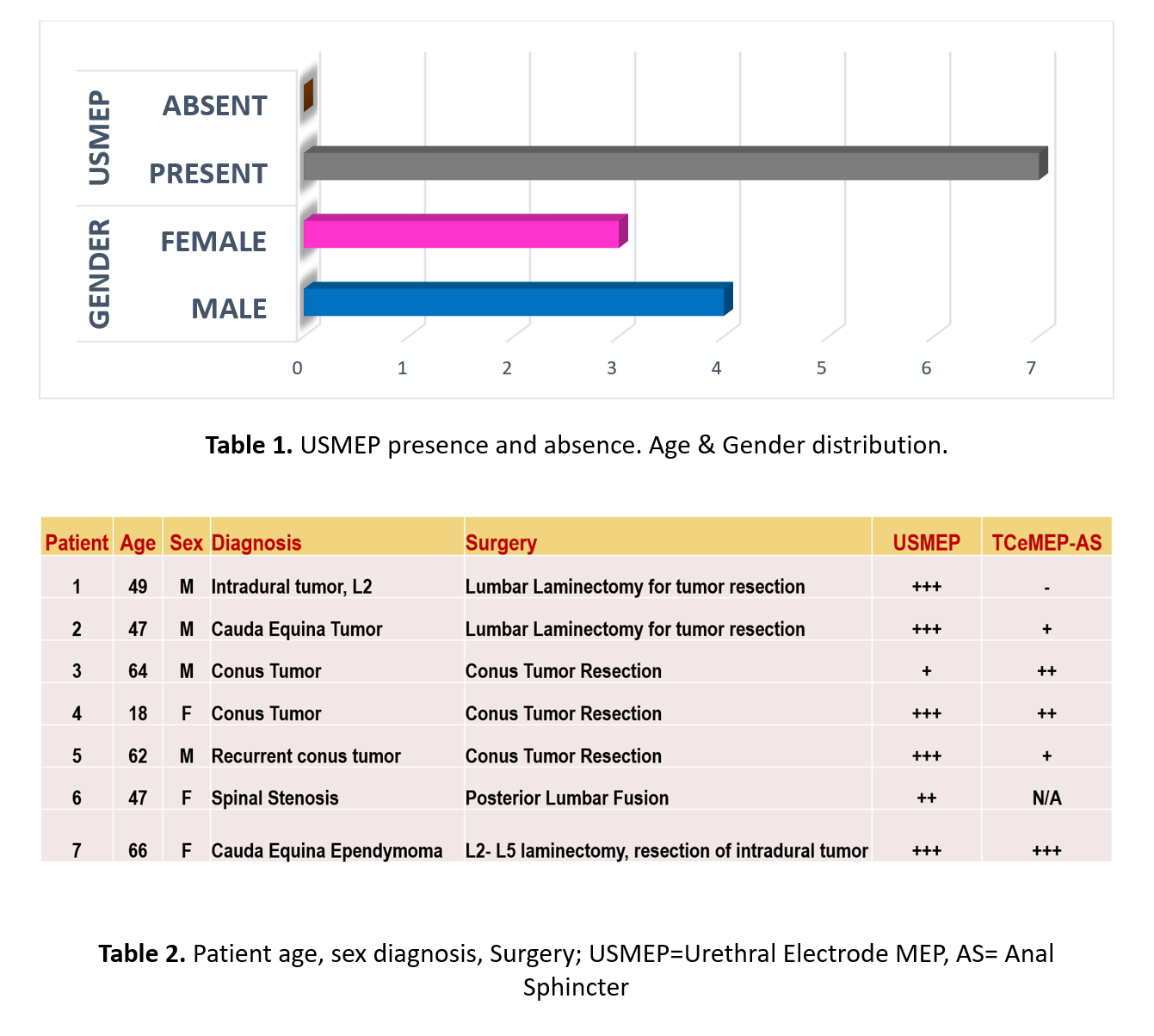
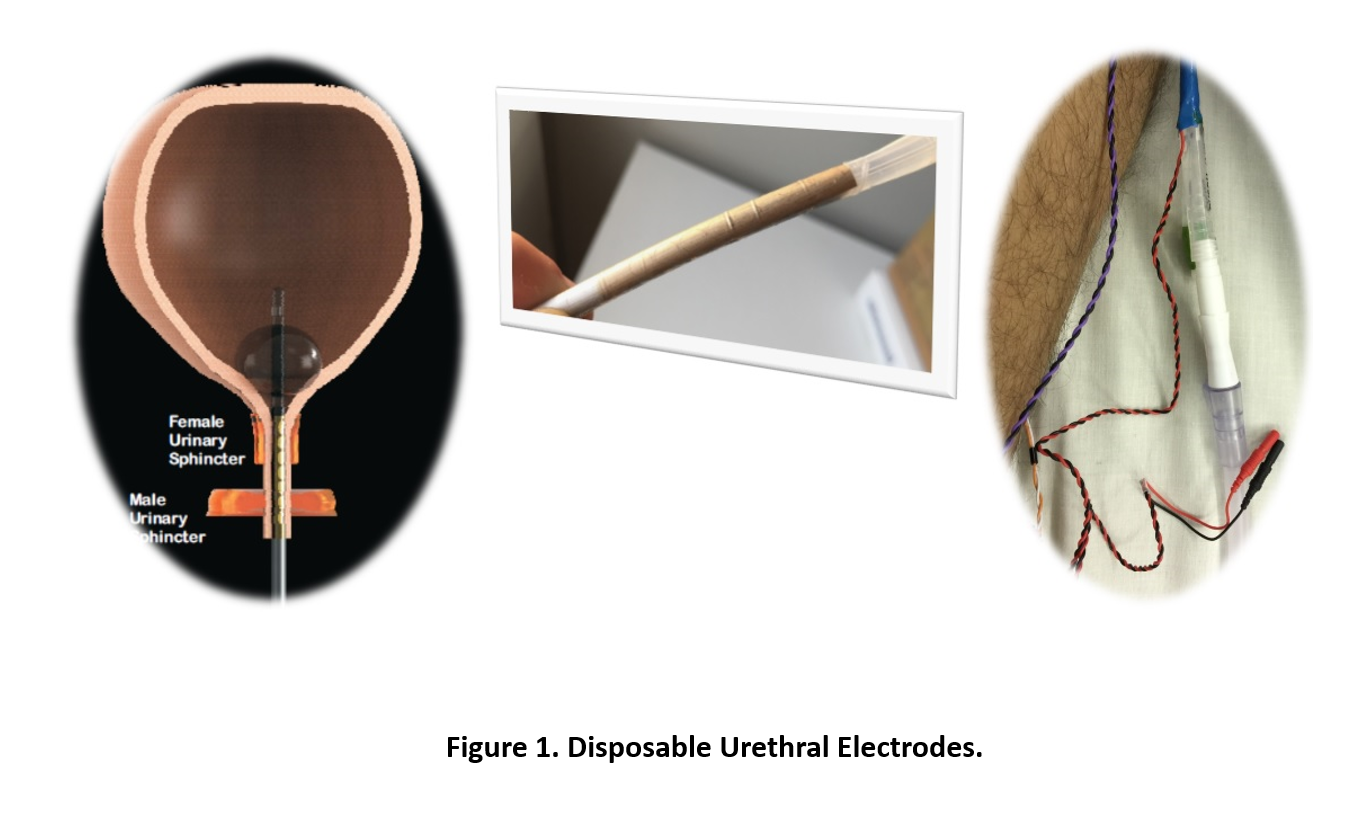
A retrospective analysis of neurophysiological monitoring data from six intradural tumors and one laminectomy for stenosis that used urethral sphincter electrodes to record USMEPs from two medical centers was performed. The patients consisted of three females and four males with ages ranging from 18 to 66 years (median: 50 years) (Tables 1&2). Four patients presented with tumors of the conus, two patients presented with intradural cauda equina tumors and one patient presented with severe spinal stenosis. Our neuromonitoring paradigm included upper and lower extremity SSEPs and MEPs, as well as spontaneous EMG from the EAS, urethral sphincter muscles (USM) and lower extremity muscles bilaterally. A catheter with urethral electrodes attached was used for recording MEPs and s-EMG from the skeletal muscle of the external urethral sphincters. Train of four (TOF) was also recorded from the Abductor Hallucis muscle as well for monitoring the level of muscle relaxant.
RESULTS:
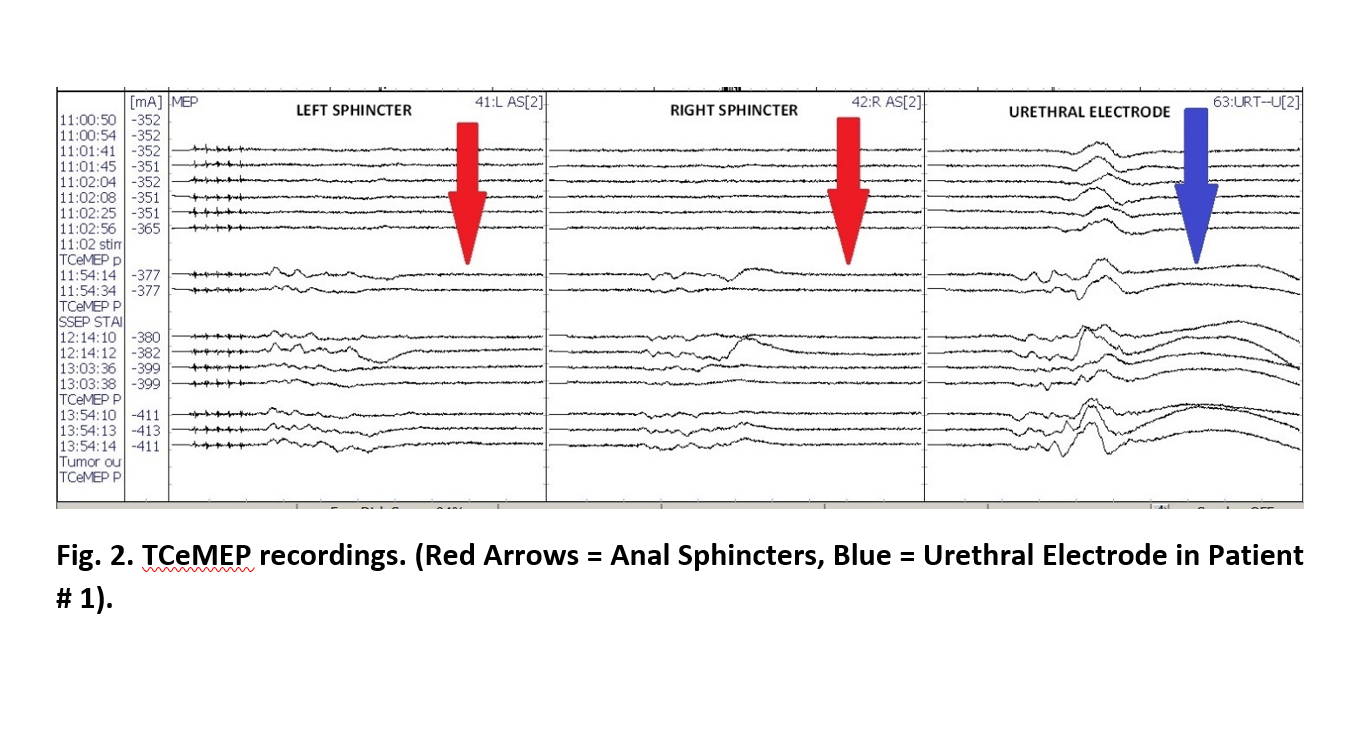
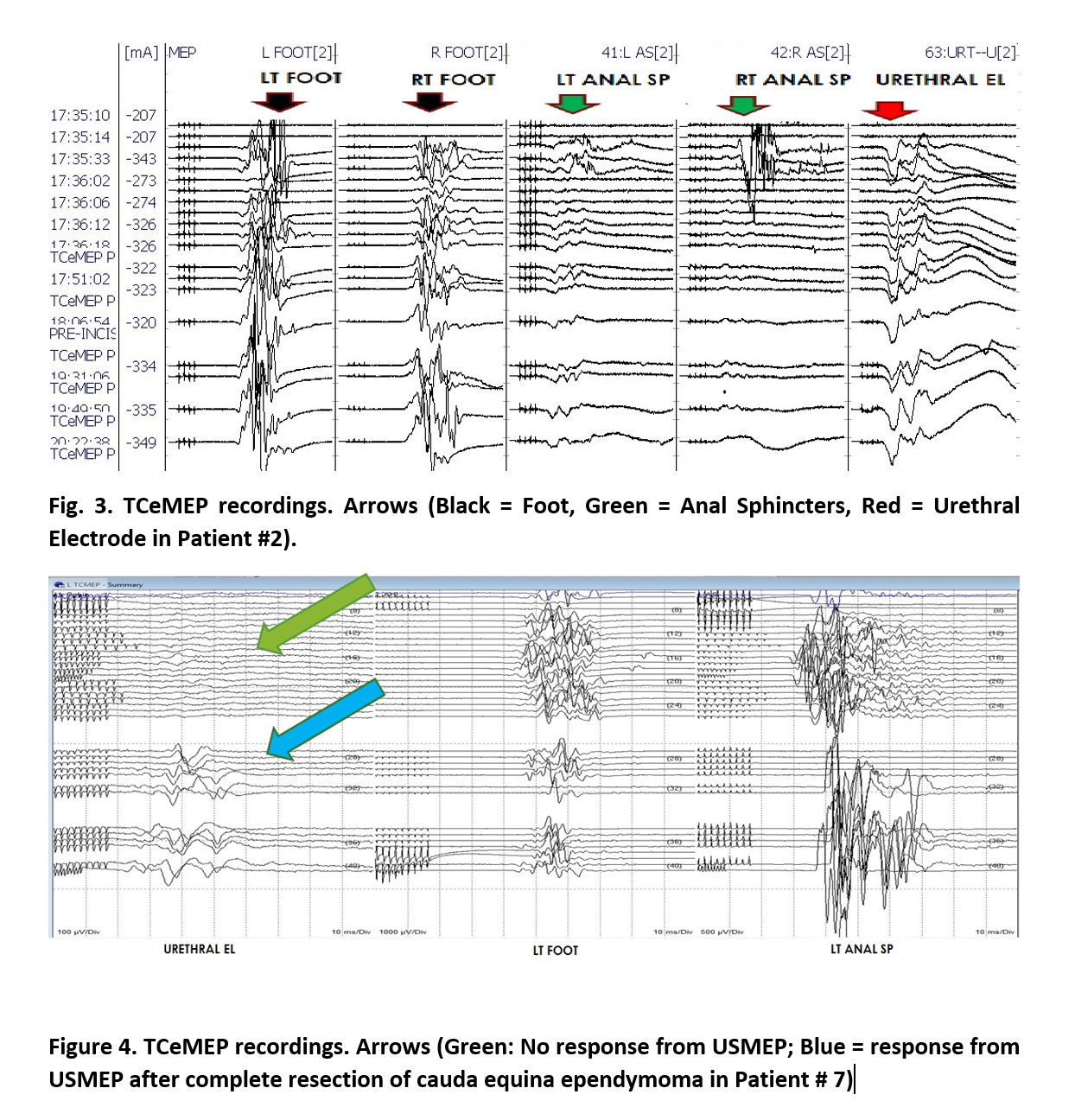
TCeMEPs were obtained from the urethral sphincters in all seven patients. The reliability of TCeMEP from the EAS was variable across all patients. In patient 7 (Fig 4), the MEP recordings from the urethral sphincter were not present at pre-incision baseline and remained absent throughout the procedure until a complete resection of the tumor was performed. At this time, immediately following tumor resection, the USMEP recordings were obtained and remained stable for the remainder of the procedure. Patient # 4 exhibited a 50% increase in amplitude of the USMEP post tumor resection as well. It is worthy to note that patients # 4 and 7 presented preoperatively with bladder incontinence, urgency and frequency. Almost immediately in the post-operative phase both patient’s frequency and urgency improved and the bladder function normalized within two weeks of having the tumor removed.
CONCLUSIONS:
In this small series, we were able to acquire motor evoked potentials in 100% of patients when recorded from the urethral sphincters using a urethral catheter with electrodes built into it. USMEPs can be attempted in surgeries that put the function of the pelvic floor at risk. Patient # 4 and 7 are illustrative cases that may show the prognostic value in using USMEPs; however, more study is needed to establish better statistical methods, better modality efficacy, and a better understanding of intraoperative countermeasures that may be employed when an alert is encountered to prevent impending neurological sequelae.
Faisal R. Jahangiri, MD, CNIM, D.ABNM, FASNM1,2,
Justin W. Silverstein, DHSc, CNIM3, Zachariah M. George, MD4, Sami Al Eissa, MD5,
1 Axis Neuromonitoring LLC, Richardson, TX, USA; 2Division of Neurology, Dept. of Medicine, King Abdulaziz Medical City, Riyadh, Saudi Arabia; 3Neuroprotective Solutions, Long Island, NY, USA. 5Division of Orthopedics, Dept. of Surgery, King Abdulaziz Medical City, Riyadh, Saudi Arabia; 4Neurological Surgery PC, Long Island, NY, USA.
Learn more about AXIS Neuromonitoring by downloading the brochure:
↓




