Triggered EMG recordings from urethral electrodes
May 03, 2019
Triggered Electromyography (t-EMG) Recordings from Urethral Electrodes
Faisal R. Jahangiri1,2* and Rabehah A. Asdi1,3
1Axis Neuromonitoring LLC, Richardson, TX, USA; 2Global Innervation LLC, Dallas, TX, USA; 3Department of Applied Cognition and Neuroscience, University of Texas, Richardson, TX, USA.
Abstract
Introduction: Multimodality Intraoperative Neurophysiological Monitoring (IONM) is routinely performed during resection for tumors of the conus, cauda equina and nerve roots. Bowel and bladder function are at risk during these procedures and are usually only monitored with EMG and/or motor evoked potentials (MEP) recorded from the external anal sphincter muscles (EAS). Unfortunately, a narrow view of pelvic floor function is provided when only analyzing the EAS which does not include the monitoring of direct bladder function. This study demonstrates the ability to acquire Triggered EMG (t-EMG) from the External Urethral Sphincter (EUS) muscles by utilizing a urethral Foley catheter with an electrode attached.
Methods: A retrospective analysis of neurophysiological monitoring data from seven intradural tumors and three tethered cord release surgeries that used urethral sphincter electrodes to record t-EMG from two medical centers was performed. The patients consisted of five females and five males with ages ranging from 8 month to 67 years (median: 49 years) (Fig 1 & 2). Our neuromonitoring paradigm included upper and lower extremity SSEPs and MEPs, as well as spontaneous & triggered EMG from the EAS, urethral sphincter muscles (USM) and lower extremity muscles bilaterally. A catheter with urethral electrodes attached was used for recording s-EMG, t-EMG and MEPs from the skeletal muscle of the external urethral sphincters (Fig 3). Train of four (TOF) was also recorded from the Abductor Hallucis muscle as well for monitoring the level of muscle relaxant.
Results: We were able to successfully record T-EMG responses from the external urethral sphincters muscles (Fig 4) in all patients (100%). It is worthy to note that only one patient presented preoperatively with bladder incontinence, urgency and frequency. Almost immediately in the post-operative phase patient’s frequency and urgency improved and the bladder function normalized within two weeks of having the tumor removed.
Conclusion: In this small series, we were able to acquire t-EMG in 100% of patients when recorded from the urethral sphincters using a urethral catheter with electrodes built into it. T-EMGs can be attempted in surgeries that put the function of the pelvic floor at risk. More study is needed to establish better statistical methods, better modality efficacy, and a better understanding of intraoperative countermeasures that may be employed when an alert is encountered to prevent impending neurological sequelae.
Keywords: Transcranial Electrical Motor Evoked Potentials; TCeMEP; Electromyographic; EMG; Neuropathy; Electrodes; Intraoperative Neurophysiological Monitoring; IONM.
_____________________________________________________________________________________
Citation: This study was presented by Dr. Faisal R. Jahangiri at the 2019 Annual Meeting of American Society of Neurophysiological Monitoring (ASNM) from May 3-5, 2019 in Chicago, Illinois.
Figure 1. Gender distribution
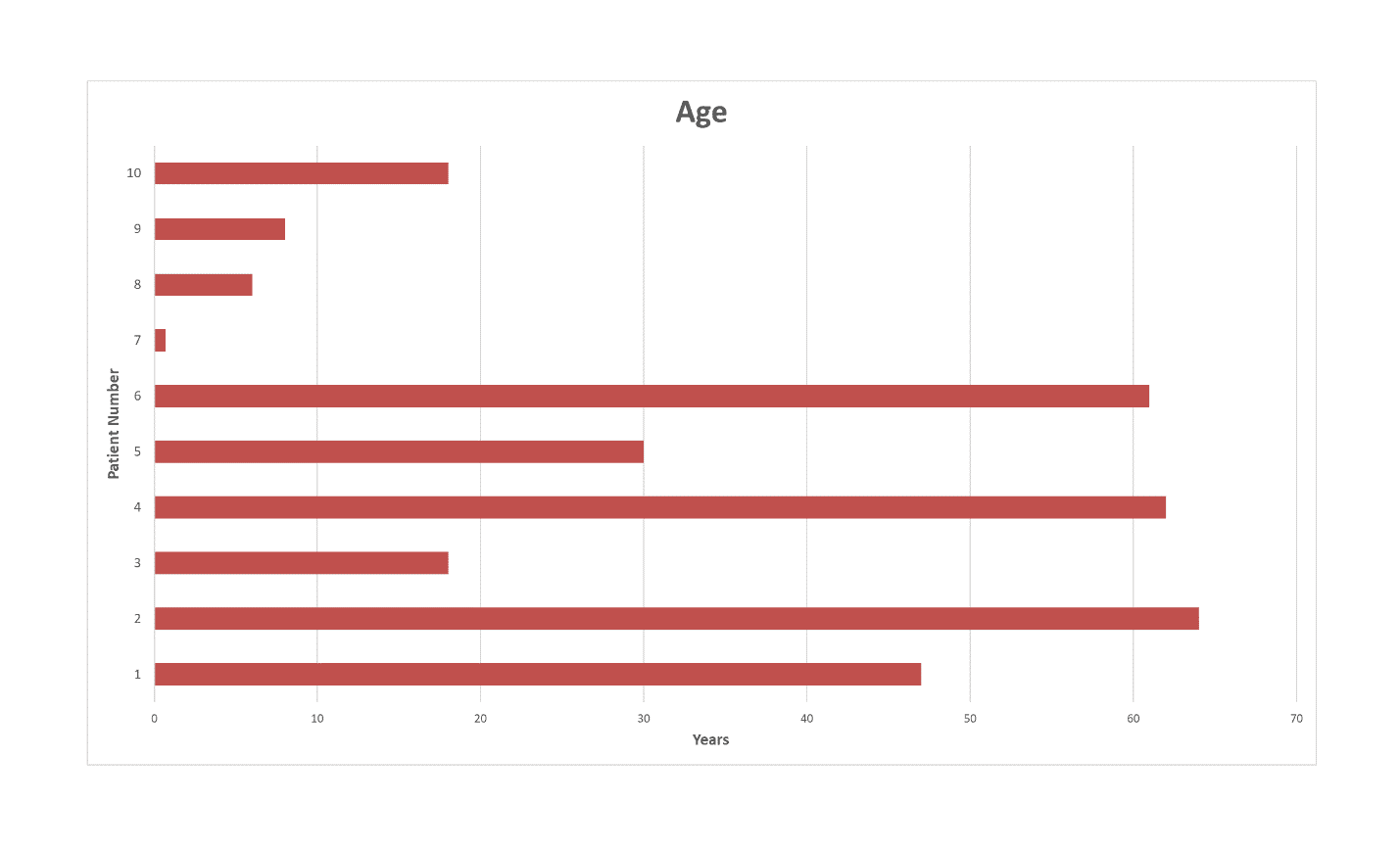
Figure 2. Age distribution

Figure 3. Disposable Urethral Electrodes.
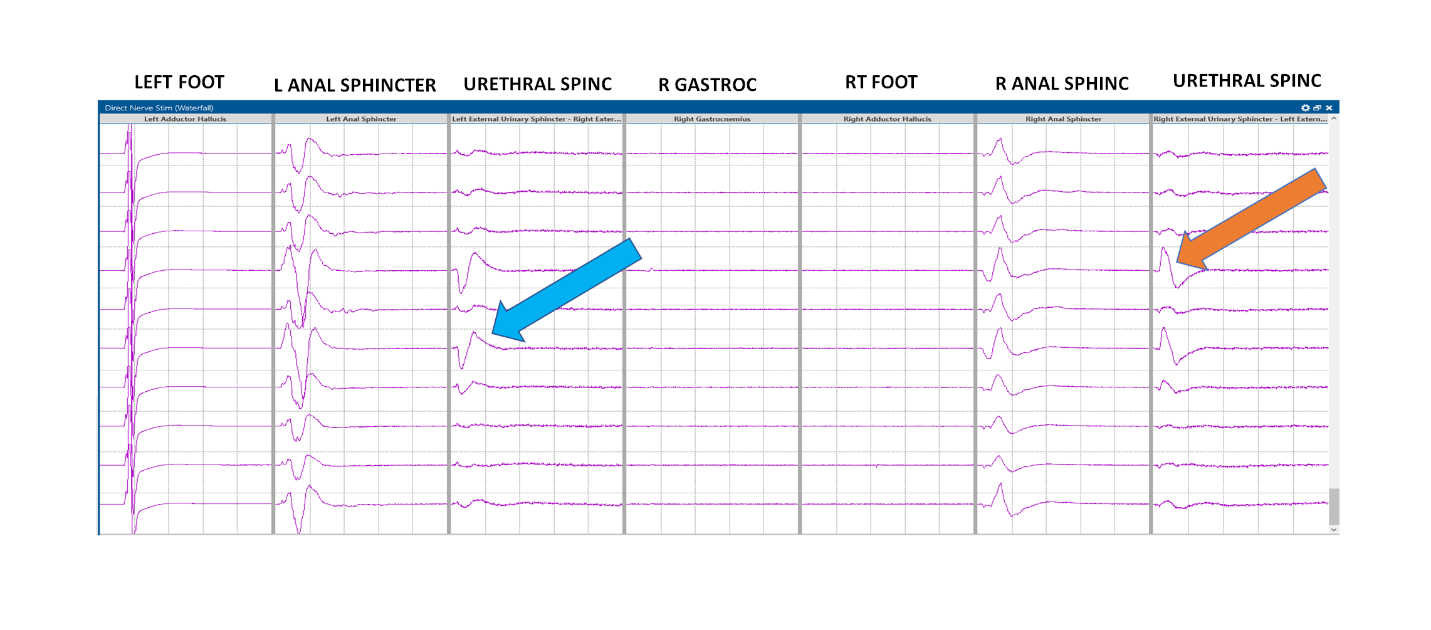
Figure 4. T-EMG recordings in Patient # 9 (Blue & Orange arrows = CMAP responses from EUS)
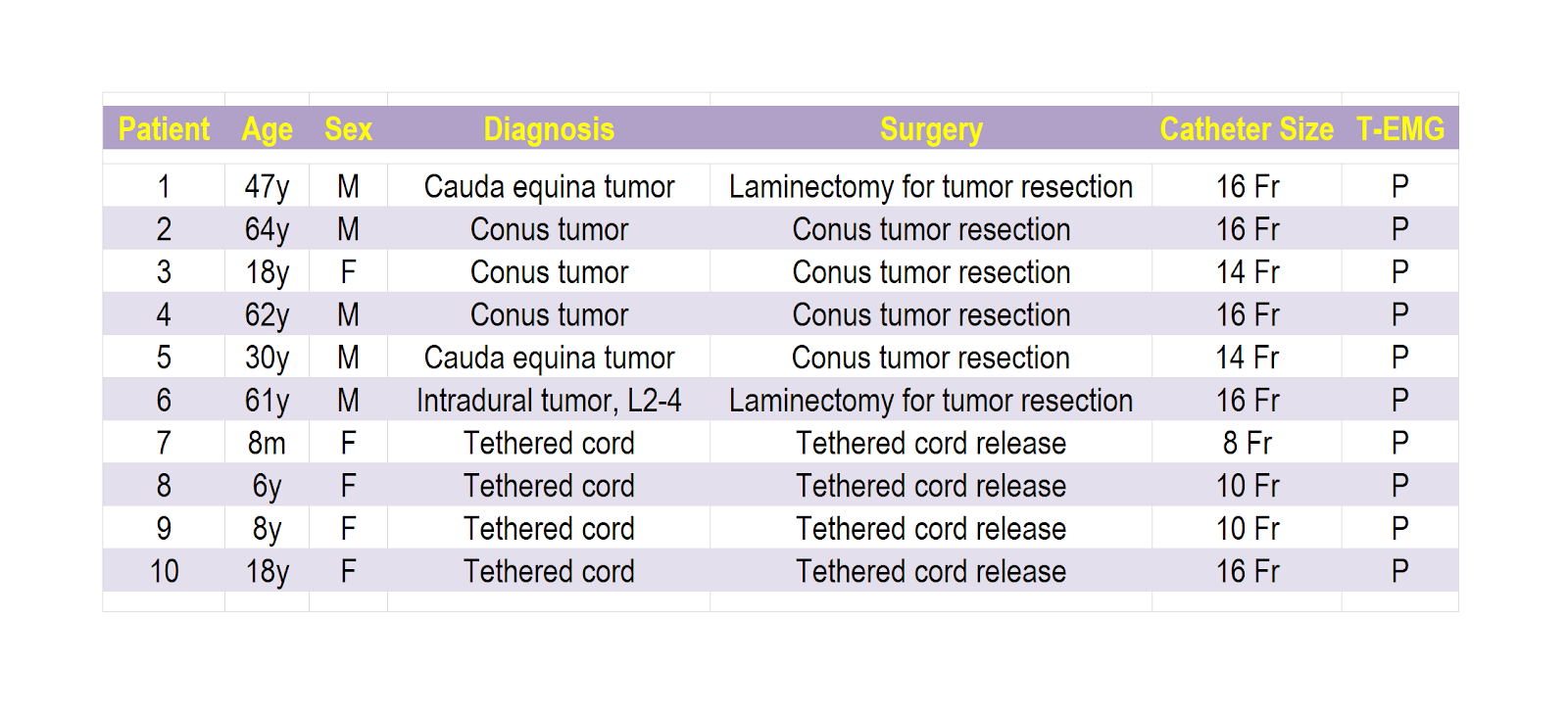
Table 1. Patient age, sex diagnosis, Surgery; Fr=Frank, Foley Catheter size; P=present t-EMG response.



