Use of Intraoperative Neurophysiological Monitoring (IONM) during Selective Dorsal Root Rhizotomy (SDR) Procedures for the Treatment of Spasticity in Patients with Cerebral Palsy
July 24, 2018
Faisal R. Jahangiri, MD, CNIM. D.ABNM, FASNM
Cerebral palsy (CP) affects movement and posture and is caused by irreversible brain damage to the motor cortex due to cerebral hypoxia before, during, or after birth up to about age three. The brain damage produces life-long disabilities. This disorder affects about one out of every 500 children worldwide. CP describes a group of permanent disorders of the development of movement and posture, causing activity limitation. In the child with cerebral palsy, due to the damage the of the motor area the brain is unable to influence the amount of muscle flexibility. The muscle command dominates the spinal cord and, as a result, the muscle is too stiff or spastic.
Spasticity is one of the most common pediatric problem managed by the hospitals, commonly seen in children with cerebral palsy, brain or spinal cord injury. Spasticity is used to describe abnormal muscle tone or muscles that have too much stiffness. Spasticity can limit movement and can interfere with daily living. Spasticity can cause debilitating complications such as deformity of the spine, contractures of joints, that can affect the patient ambulation. Spasticity is associated with diplegic, quadriplegic or hemiplegic CP.
Spasticity is treated to minimize its adverse effect on the musculoskelatal system. The adverse effects of spasticity include inhibition of movement and muscle growth resulting in tissues and joint deformities. In a patient with spasticity, due to the abnormal signals sent from the muscles to the spinal cord and back again, the muscles contracts and do not relax appropriately.
Patients with CP have several treatment options, such as medical, rehabilitation, surgical. The treatment selection is dependent on the patient’s age, severity, and available expertise, etc.
Selective dorsal root rhizotomy (SDR): SDR has been used effectively in the treatment of spasticity in some children with cerebral palsy. SDR is a neurosurgical procedure that involves selectively sectioning (cutting) of some of the sensory (dorsal) nerve fibers with abnormal responses that enter the spinal cord and synapse with lower motor neurons. The SDR technique can be used under electrophysiological guidance in a patient with cerebral palsy for successful treatment of spasticity.
Intraoperative Neurophysiological Monitoring (IONM) :
A multimodality IONM approach with Somatosensory Evoked Potentials (SSEP), Transcranial electrical Motor Evoked Potentials (TCeMEP) and Electromyography (EMG) is recommended during SDR procedures. Baselines responses are recorded after intubation and before incision under general anesthesia. The spontaneous (s-EMG) and triggered EMG (t-EMG) can be effectively used intraoperatively for selection of dorsal rootlets. Rootlets with abnormal EMG firing patterns are cut in patients diagnosed with cerebral palsy for the reduction of muscle spasticity.
Method and Setup
Anesthesia: General anesthesia with Total Intra Venous Anesthesia (TIVA), Propofol, Fentanyl or Remifentanil infusion, is highly recommended. The neuromuscular blockade should be used only for initial intubation. Subsequent neuromuscular blockade levels are monitored with a train of four (TOF 4/4) from foot muscles. A 4/4 twitch is maintained for accurate monitoring.
IONM Modalities:
Somatosensory Evoked Potentials (SSEP)
Transcranial electrical Motor Evoked Potentials (TCeMEP)
Spontaneous EMG (s-EMG)
Triggered EMG (t-EMG)
Train of Four (TOF)
Muscles Selection: From L2 to S4 roots (Adductor Brevis, Quadriceps, Tibialis Anterior, Medial Gastrocnemius, Abductor Hallucis, Extensor Hallucis Brevis and Anal Sphincters muscles).
Procedure:
SDR begins with a 1-2-inch incision along the center of the lower back just above the waist. An L1 laminectomy is performed, to expose the spinal cord and the spinal nerves (L2-S1) underneath. Ultrasound and an x-ray locate the tip of the spinal cord, where there is a natural separation between sensory and motor nerves. A rubber pad is then placed to separate the motor from the sensory nerves. The sensory (dorsal) nerve roots are wrapped individually in a pad, above the motor roots and away from the operative field. After the sensory nerves are exposed, each sensory nerve root is divided into 3-5 rootlets. T-EMG is used to identify and separate the dorsal roots from the ventral roots. Dorsal nerve rootlets with abnormal responses are identified and sectioned. Each rootlet is tested with t-EMG. A single pulse technique is used for the identification of each sensory root. Followed by a 50 Hz train t-EMG from 0.05-5.0 mA for the stimulation of individual nerve rootlets. Each rootlet is graded from 0 (mild) to 4 (severe) for spasticity. The severely abnormal rootlets (only Grade 3 and 4) are sectioned. This technique is repeated bilaterally for all rootlets between spinal nerves L2 and S2.
Selective Dorsal Root Rhizotomy (SDR) is an effective treatment of spasticity in lower extremities. Almost all spastic diplegics patients benefit from SDR. IONM can be used effectively to guide the neurosurgeon in selecting the dorsal rootlets with abnormal muscle contraction for rhizotomy. Postoperatively the patient needs physiotherapy for rehabilitation.
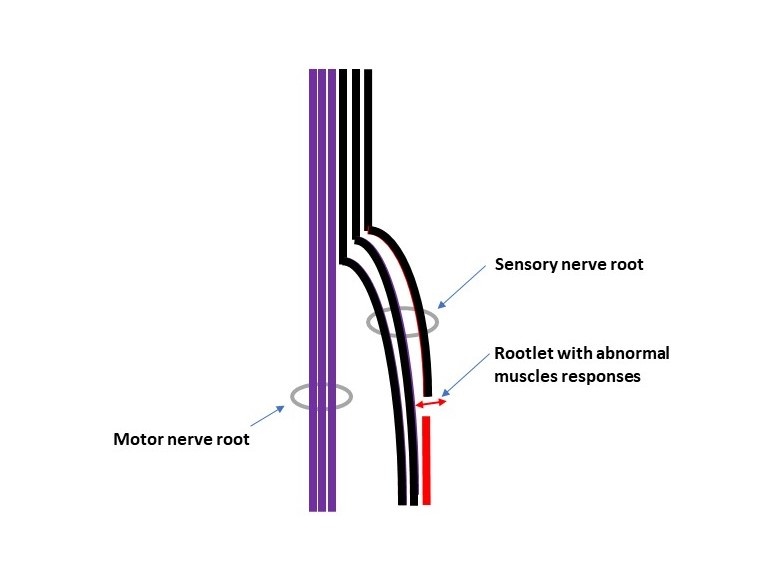
Fig 1. Selective Dorsal Root Rhizotomy (SDR): Cut Dorsal Rootlet.
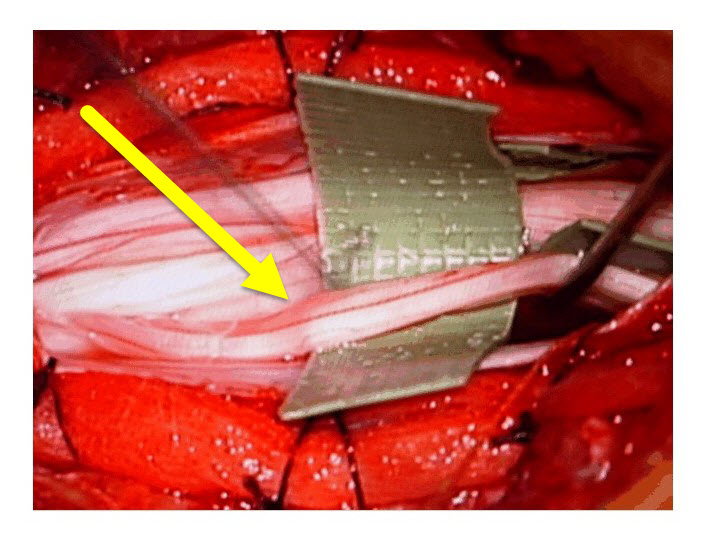
Fig 2. Selective Dorsal Root Rhizotomy (SDR): Separating the Dorsal Rootlets.

Fig 3. Selective Dorsal Root Rhizotomy (SDR): 50 Hz Stimulation with Grade 0/1 responses.
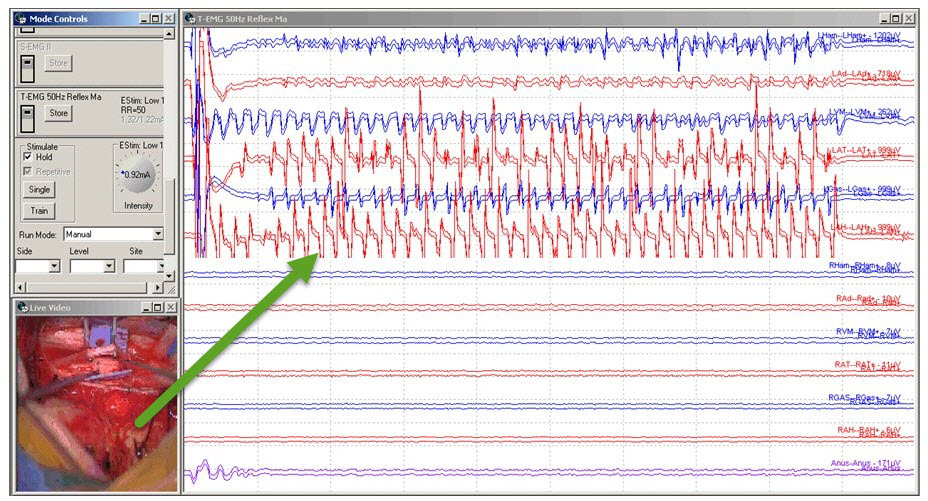
Fig 4. Selective Dorsal Root Rhizotomy (SDR): 50 Hz Stimulation with Grade 3 responses. Left: Video from the microscope with rootlet stimulation.
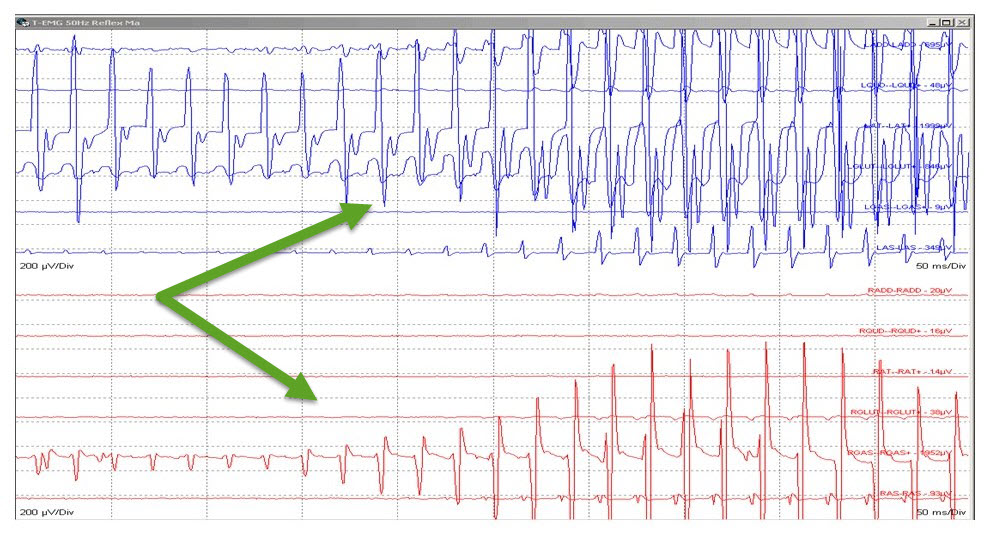
Fig 5. Selective Dorsal Root Rhizotomy (SDR): 50 Hz Stimulation with Grade 4 responses.
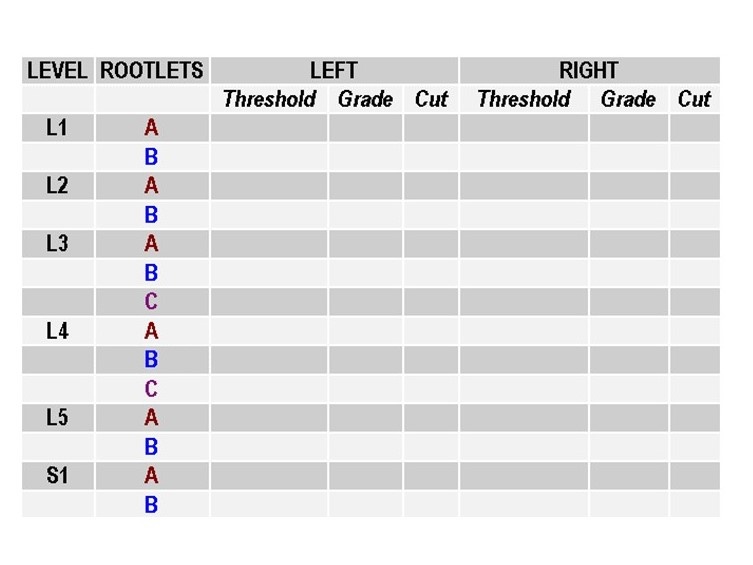
Fig 6. Selective Dorsal Root Rhizotomy (SDR): Grading Sheet Sample.



