External Cerebrospinal Fluid Drainage in the Management of Nonaneurysmal Subarachnoid Hemorrhage
By Admin | March 25, 2022
Abstract
Distinguishing the aneurysmal from nonaneurysmal subarachnoid hemorrhage (SAH) may be difficult as acute bleeding in the subarachnoid space is a common denominator. It is believed that toxic effects of breakdown products of acute bleed, including hemoglobin, contribute to the morbidity and mortality of this condition; and that early drainage will potentially reduce them. This series focuses on our local experience with the application of external cerebrospinal fluid (CSF) drainage in the management of a series of cases confirmed to be nonaneurysmal SAH and its effects on the outcome. The objective of this report is to observe the usefulness of external CSF drainage in the management of nonaneurysmal SAH. Five consecutive cases over four years were reviewed and reported as a case series. The main points we focused on were presentation, diagnostic findings on imaging, CSF drainage, and outcome up to six months. All the patients presented with headaches described as sudden, and only one had significant impairment of consciousness Glasgow Coma Scale (GCS) 10/15. Three out of the five patients had a premorbid hypertensive condition of unclear control status. We also observed that three out of the five had a low-pressure pretruncal/perimesencephalic pattern of bleed, whereas two had the typical high-pressure SAH pattern. CT angiography (CTA) was negative in all. Four had lumbar drainage, while one had external ventricular drainage. All were discharged within three weeks and functioned optimally at six months. CSF drainage in managing nonaneurysmal SAH is achievable with minimal access procedures, including lumbar drain (LD) and external ventricular drainage (EVD), which may have further reduced the low morbidity normally associated with this condition.
Introduction
Clinical presentation of subarachnoid hemorrhage is often sudden, and the management is even more challenging, especially in a resource-poor setting. There is presently not a lot of local data and experience in the contemporary management of this inherently fatal form of stroke in our practice environment [1]. Nonaneurysmal type subarachnoid hemorrhage (SAH) has a lower rate of mortality and morbidity in comparison to the aneurysmal type. Irrespective of the type of SAH, they both have a challenge of an unusual amount of fresh blood in the subarachnoid space, which has been implicated in the emergence of complications such as cerebral vasospasm. This results in poor outcomes, especially in aneurysmal types and also, to a lower extent, in nonaneurysmal ones. Although the pathophysiological mechanisms of vasospasm are yet to be fully understood, we currently know that breakdown products of hemoglobin play a major role in this process [2]. It has also been observed that the incidence of vasospasm shows a close correlation with volume, density, and persistence of clots in the subarachnoid space and ventricular cavities [3]. In line with this idea, it has been suggested that early surgical removal of these clots may reduce the frequency and severity of vasospasms [4]. The bleed and its broken-down products are usually mixed with cerebrospinal fluid (CSF) at various concentrations depending on the volume of the bleed. Therefore, drainage of the CSF is a pragmatic way of cleansing the subarachnoid space of these bloodstains. This is also facilitated by the fact that fresh CSF is constantly produced and circulated at an average rate of 20ml/hour.
Several methods of CSF drainage have been reported, including external ventricular drainage, continuous lumbar drainage, and cisternal drainage with microsurgical fenestration of the lamina terminalis. The latter technique was recently reported but abandoned as it was shown to have no benefits [5]. An external ventricular drain (EVD) is useful in the drainage of CSF containing breakdown products of hemoglobin; however, this technique has been associated with an increased risk of developing ventriculitis and posthemorrhagic hydrocephalus [6]. Lumbar drainage (LD) is an alternative and has lower rates of hemorrhagic, obstructive, and infectious complications than ventricular drainage, and its use in patients with SAH is based on evidence provided by Macdonald [7] and Hänggi et al. [8]. These authors found that CSF drainage may reduce the incidence and potential consequences of vasospasms [7,8]. Some studies have revealed that due to gravitational forces, the concentration of blood components in CSF in patients with SAH is greater when CSF is collected using an LD than with an EVD. This proves that blood products accumulate mainly in the lumbar and basal cisterns [9]. These findings indicate that draining CSF from the lumbar cistern allows for more efficient clearance of breakdown products of hemoglobin from CSF and may therefore have detectable clinical benefits.
Two distinct hemorrhage patterns have been described radiologically in the nonaneurysmal SAH: an aneurysmal hemorrhage pattern with no identifiable aneurysm on angiography and the pretruncal/perimesencephalic hemorrhage pattern [10]. Regardless of the cause of bleed, it is currently known that breakdown products of hemoglobin play a major role in the process of vasospasm which shows a close correlation with volume, density, and persistence of clots in the subarachnoid spaces and ventricular cavities. It is hoped that early deployment of external CSF diversion/drainage through external ventricular drainage or continuous lumbar drainage will encourage the early cleansing of the subarachnoid spaces, with an earlier resolution of symptoms in this category of patients and their subsequent return to normal activities. Following appropriate clearance from the institutional ethical review board and consent from patients, this report presents a concise review of a series of five patients, and the experiences gathered therefrom are hereby shared.
Case Presentation
Case 1
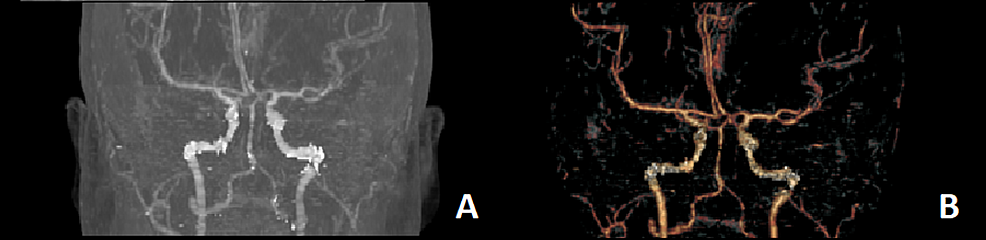
A 34-year-old woman was referred from another facility on account of a one-week history of sudden onset of severe headache, blurring of vision, and episodes of projectile vomiting. There was no history of recent head trauma. She later described the onset of the headache as the worst headache of her life. She had been diagnosed with hypertension since her first pregnancy 10 years ago. In the ED, her blood pressure was 140/97mmHg. Pain visual analog score (VAS) was 9/10. An urgent CT of the brain demonstrated acute SAH in the prepontine and perimesencephalic cisterns, without extension into the sylvian or interhemispheric fissures. There was no intraventricular or intraparenchymal hemorrhage (Figure 1). CT angiography (CTA) did not reveal any aneurysms (Figure 2).
Her physical examination was notable for a right abducens palsy with nuchal tenderness. She was restless, in painful distress, but was conscious, obeyed commands, and was oriented to time, place, and person. She was unable to count fingers on the...(More)
For more info please read, External Cerebrospinal Fluid Drainage in the Management of Nonaneurysmal Subarachnoid Hemorrhage, by Cureus